What families need to know about Acute Flaccid Myelitis
Acute flaccid myelitis (AFM) is a rare but serious condition. It affects the nervous system, specifically the area of the spinal cord called gray matter, which causes the muscles and reflexes in the body to become weak. This condition is not new. However, the large number of AFM cases reported since 2014, when we first started our surveillance for this condition, is new. The risk of getting AFM varies by age and year. We have seen increases in AFM cases every two years since 2014 and mostly in young children. Still, CDC estimates that less than one to two in a million children in the United States will get AFM every year. Since 2014, most patients (more than 90%) had a mild respiratory illness or fever consistent with a viral infection before they developed AFM. All the stool specimens from AFM patients that we received tested negative for poliovirus. We are working closely with national experts to better understand the possible causes of AFM and update our information on treatment.
Symptoms
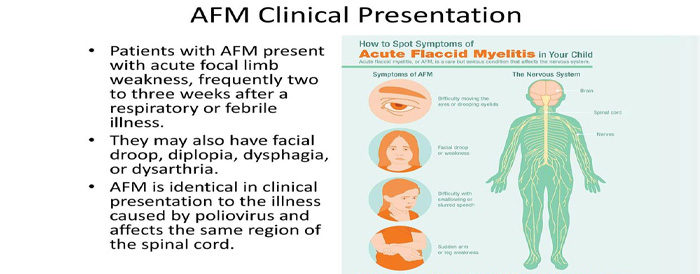
Most people will have sudden onset of arm or leg weakness and loss of muscle tone and reflexes. Some people, in addition to arm or leg weakness, will have:
- facial droop/weakness,
- difficulty moving the eyes,
- drooping eyelids, or
- difficulty with swallowing or slurred speech.
Numbness or tingling is rare in people with AFM, although some people have pain in their arms or legs. Some people with AFM may be unable to pass urine (pee). The most severe symptom of AFM is respiratory failure that can happen when the muscles involved with breathing become weak. This can require urgent ventilator support (breathing machine). In very rare cases, it is possible that the process in the body that triggers AFM may also trigger other serious neurologic complications that could lead to death.
If you or your child develops any of these symptoms, you should seek medical care right away. Your doctor may collect information about your symptoms and send this information to their health departments. This is because CDC is asking doctors to be alert for patients with symptoms of AFM so that we can learn more about this condition.
Diagnosis
For parents who have a child with AFM
CDC understands that parents who have had a child diagnosed with AFM have many concerns and questions. AFM is a serious condition that can be difficult for children and their parents or caregivers. You are in the best position to be an advocate for your child. Talk to the doctor about any discomfort your child may have and ask about treatment options. Ask your child’s school about resources they may have to accommodate this illness. Spending time with others is also an important part of wellbeing and recovery. Encourage friends and family to spend time with your child if they feel well enough for visitors.
AFM is diagnosed by examining a patient’s nervous system in combination with reviewing pictures of the spinal cord. A doctor can examine a patient’s nervous system and the places on the body where he or she has weakness, poor muscle tone, and decreased reflexes. A doctor can also do an MRI (magnetic resonance imaging) to look at a patient’s brain and spinal cord, do lab tests on the cerebrospinal fluid (the fluid around the brain and spinal cord), and may check nerve conduction (impulse sent along a nerve fiber) and response. It is important that the tests are done as soon as possible after the patient develops symptoms.
AFM can be difficult to diagnose because it shares many of the same symptoms as other neurologic diseases, like transverse myelitis and Guillain-Barre syndrome. With the help of testing and examinations, doctors can distinguish between AFM and other neurologic conditions.
Learn more about the type of information that helps to determine if a patient has AFM or not.
Possible Causes of AFM
Certain viruses are known to cause AFM including enteroviruses, such as poliovirus and enterovirus A71 (EV-A71), and West Nile virus. Since 2014, most patients with AFM (more than 90%) had a mild respiratory illness or fever consistent with a viral infection before they developed AFM. All the stool specimens from AFM patients that we received tested negative for poliovirus. Most patients had onset of AFM between August and October, with increases in AFM cases every two years since 2014. At this same time of year, many viruses commonly circulate, including enteroviruses, and will be temporally associated with AFM.
We detected coxsackievirus A16, EV-A71, and EV-D68 in the spinal fluid of four of 440 confirmed cases of AFM since 2014, which points to the cause of their AFM. For all other patients, no pathogen (germ) has been detected in their spinal fluid to confirm a cause. When a pathogen (germ) is found in the spinal fluid, it is good evidence that it was the cause of a patient’s illness. However, oftentimes, despite extensive testing of AFM patients, no pathogens are found in the spinal fluid. This may be because the pathogen has been cleared by the body or it is hiding in tissues that make it difficult to detect. Another possibility is that the pathogen triggers an immune response in the body that causes damage to the spinal cord. We are searching for what triggers AFM in some children who have had a fever and/or respiratory illness compared to most children who don’t get AFM.
Treatment
There is no specific treatment for AFM, but a doctor who specializes in treating brain and spinal cord illnesses (neurologist) may recommend certain interventions on a case-by-case basis. For example, neurologists may recommend physical or occupational therapy to help with arm or leg weakness caused by AFM. CDC is working closely with national experts to better understand how to treat AFM and update our clinical management considerations. We are also working to understand the long-term outcomes (prognosis) of people with AFM.
Prevention
Since we don’t know the cause of most of these AFM cases or what triggers this condition, there is no specific action to take to prevent AFM.
Certain viruses are known to cause AFM including enteroviruses, such as poliovirus and enterovirus A71 (EV-A71), and West Nile virus.
You can protect yourself and your children from poliovirus by getting vaccinated. Polio vaccine contains inactivated (not live) virus, and protects against poliovirus. This vaccine does not protect against other viruses that may cause AFM.
You can protect against bites from mosquitoes, which can carry West Nile virus, by using mosquito repellent, staying indoors at dusk and dawn (when bites are more common), and removing standing or stagnant water near your home (where mosquitoes can breed).
You can protect yourself and others from enteroviruses by washing your hands often with soap and water, avoiding close contact with people who are sick, and cleaning and disinfecting frequently touched surfaces, including toys.
For more information on what CDC is doing, see our AFM Investigation page.

